Sorensen Clinic
Plastic and Reconstructive Surgery
10 Knaresborough Place
Kensington
London SW5 0TG
United Kingdom
Appointments: +44 (0) 20 7600 4444
Email: info@sorensenclinic.com
Office hours
Monday - Friday: 09.00 - 17.30
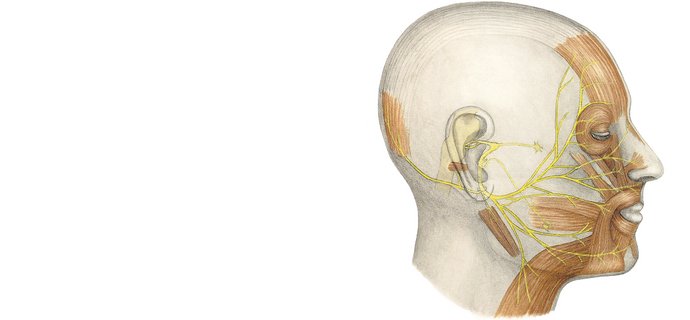
There are a range of symptoms of lasting facial paralysis: for example, the forehead on the paralysed side of the face is unable to raise the eyebrow, causing descent of brow and soft-tissues (ptosis). Although the lid can open, it may have difficulty closing, leading to prolonged exposure of the eye (corneal dryness). The cheek and mouth may also droop, resulting in problems eating and drinking (oral incompetence) and the inability to smile on the affected side.
Depending on the extent and duration of the paralysis, a number of dynamic and static procedures may be employed to alleviate these problems.
In long-lasting facial paralysis (>18 months), muscles undergo atrophy due to lack of nerve stimuli and cannot regain function. In order to re-establish voluntary facial movements (a symmetric smile), viable muscle must be transplanted into the paralysed side of the face. This procedure known as “facial reanimation” or “dynamic reconstruction” detaches nerves and muscles from the leg/body, and reattaches them into the paralysed area. The procedure (performed in two stages) is designed to permit healthy nerves from the non-paralysed side to gain control over the transplanted muscles in the paralysed side (cross-facial nerve graft). In some cases facial palsy may affect both sides of the face (Moebius syndrome), which requires even further specialised treatment regimes.
A number of surgical procedures targeting specific problems such as tightening of the oral commissure, brow lifts and eyelid surgery (implantation of platinum chains or gold weights in upper eyelids and tightening of lower lid), offer temporary to long-lasting improvement, either as stand-alone procedures or in combination. The choice of procedure is complex and demands examination and discussion.
Dynamic procedures require young to middle aged patients in good health, who are motivated to undergo repeated surgeries and long facial re-education/rehabilitation. For a child with congenital facial palsy, the condition is best treated around the age of 5-6 years. Generally, early surgery is not necessary unless eye exposure is a problem, in which case surgery can be done at any age. Static procedures may offer instant improvement to most patients with facial palsy, regardless of age.
Dr Sorensen's recommended treatments include
● Facial reanimation (smile surgery)
First stage: cross-facial nerve graft. Second stage (6-9 months later): transplantation of muscle tissue (free functional muscle transfer) harvested from the pectoralis minor muscle, the gracilis muscle or the latissimus dorsi muscle.
● Static procedures
Fascial slings (fascia latae) secure the position of the mouth and corner of the nose.
Facelift for improved symmetry.
Brow lift for correction of ptosis.
Soft-tissue restoration by lipodermal grafts and fat grafting.
Facial implants.
Perioral soft-tissue enhancement and upper lip repositioning.
Botox for asymmetries, facial synkinesis and muscle spasms.
Platinum chain or gold weight insertion (treatment of lagophthalmos).
Lateral tarsorraphy (symptomatic relief from corneal exposure).
Canthopexy.
Canthoplasty.
Lower eyelid fascial sling (palmaris longus).
Treatment for asymmetric facial atrophy and hollowness.
Adjustment of eyelid tissues (blepharoplasty).